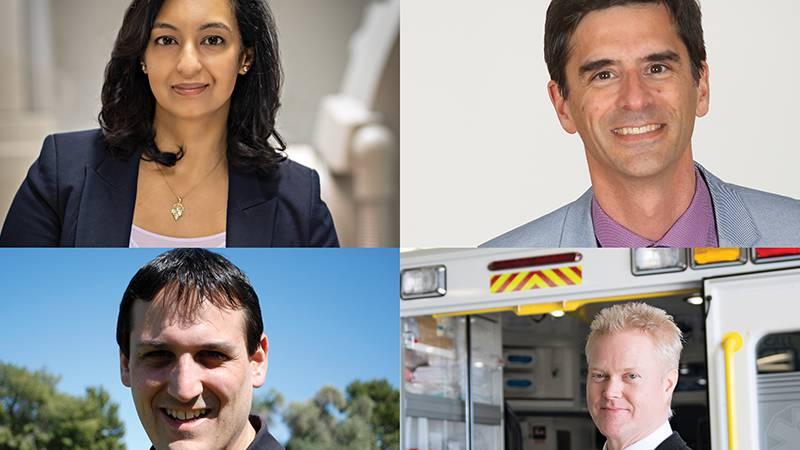
Dr. Ratika Parkash (upper left), director of research and heart rhythm in the division of cardiology; Dr. John Sapp (upper right), QEII cardiologist and the assistant dean of clinical research for Dalhousie University’s faculty of medicine; Judah Goldstein (lower left), research co-ordinator with EHS; and Dr. Andrew Travers (lower right), the provincial medical director for EHS, are collaborating on research to investigate how Nova Scotia’s pandemic response has affected morbidity and mortality
QEII study looks at impact of COVID-19 pandemic on cardiac health
Originally published on qe2times.ca.
The number of deaths directly caused by COVID-19 has been well documented, both in Nova Scotia and across the country. What’s less examined is the number of deaths indirectly caused by the pandemic.
For example, did cardiac and stroke deaths in Nova Scotia increase because people did not seek emergency care during the lockdown?
This is one of the questions Dr. Ratika Parkash, director of research and heart rhythm in the division of cardiology at the QEII Health Sciences Centre, is attempting to answer with the study titled Physical Distancing and Medical Distancing: Reducing the Cardiac and Neurovascular Impact of COVID-19.
“As soon as the lockdown began, people stopped coming to the emergency department,” says Dr. Parkash.
While cardiac disease is a silent killer, there are clearly defined symptoms that precede an episode of cardiac arrest.
“If you ignore those symptoms and don’t go to the hospital, then bad things will happen,” says Dr. Parkash. Symptoms that are normally simple to treat can lead to severe consequences that could be avoided if treated at the right time.
With $73,750 in funding, Dr. Parkash and her team are investigating how Nova Scotia’s pandemic response has affected morbidity — disease symptoms — and mortality in patients with known or new onset cardiovascular or neurovascular disease.
The study is funded by the Nova Scotia COVID-19 Health Research Coalition, which is a collaborative partnership between Nova Scotia Health, the QEII Foundation, Dalhousie University, Dalhousie Medical Research Foundation, IWK Foundation, IWK Health Centre, Dartmouth General Hospital Foundation, and Research Nova Scotia. This coalition committed $1.5 million to support the Nova Scotia research community on COVID-19 related projects.
“There was a spike in out-of-hospital deaths from cardiac arrest in many jurisdictions around the world during the first months of the COVID-19 lockdown,” says co-investigator Dr. John Sapp, QEII cardiologist and the assistant dean of clinical research for Dalhousie University’s faculty of medicine.
“We were concerned that the contraction of medical services and the fear of COVID-19 in the community was preventing people here in Nova Scotia from seeking care when they needed it,” says Dr. Sapp.
The study’s authors also wanted to know what is happening to patients who were waiting for surgery that was postponed during the lockdown. There were hundreds of patients on waiting lists for valve surgery or bypass surgery when all elective procedures were shut down across the province.
“We want to know what effect this had on patients and if it increased mortality and morbidity,” says Dr. Parkash. “Having this information will help us better allocate resources in future waves of COVID-19. For example, rather than a blanket shutdown, we would be able to target those areas where there are least likely to be negative consequences.”
Data gathered so far indicates that acuity — the severity of illness and symptoms presented by patients in emergency departments — did increase during the lockdown period from mid-March to late May 2020.
“We were seeing patients waiting too long at home and coming in much more sick than would have otherwise been the case,” says Dr. Parkash.
Data is still being gathered for the period from May to the end of October, she adds. This will provide insight on patients with less acute symptoms who did not seek treatment, either from their family physician or at the emergency department.
“We wanted to look at this systematically, so when facing a second or third wave, we can minimize harm and maximize safety for patients,” says Dr. Sapp.
To get a better picture on outcomes for people suffering out-of-hospital cardiac arrest, the study authors partnered with Emergency Health Services (EHS) Nova Scotia.
Judah Goldstein, research co-ordinator with EHS, says the results will help decision makers with future public health emergencies, particularly with regards to getting the right messages to the public.
“We’re interested in learning if there were unintended consequences about the messaging that went out about COVID-19,” says Judah. “The findings should help inform decision makers on their messaging about the safety of calling 911 or going to emergency.”
EHS was able to bring its wealth of research expertise and data to the study. Dr. Andrew Travers, the provincial medical director for EHS, is excited about the opportunity to have cardiologists working directly with front-line paramedics on a research project.
“We’re breaking down silos with this collaboration between the in-hospital system of care and the out-of-hospital system,” says Dr. Travers. “It creates opportunities for bidirectional data flow.”
The study’s authors want to get the message out that hospital emergency rooms are safe to visit during the pandemic. Visitors are screened before entering and procedures have been changed to ensure patients are not moving through multiple areas.
“Hospitals are taking every precaution to ensure that visitors are not going to contract COVID-19,” says Dr. Parkash. “Yes, COVID-19 is a serious issue. But if you have these symptoms, then you should not delay getting treatment.”